The Institute of Medicine (IOM) historic 2011 report, Relieving Pain in America, documented the profound cumulative impact of chronic pain on our nation. Findings indicated that four in ten American adults live with chronic pain disorders, with annual costs exceeding $500 billion. The IOM report noted the increasing recognition and importance of a cluster of pain conditions that frequently occur together and predominantly affect women. These disorders, recently termed by the U.S. Congress and National Institutes of Health as Chronic Overlapping Pain Conditions (COPCs), include: vulvodynia, temporomandibular disorders (TMD), myalgic encephalomyelitis/chronic fatigue syndrome, irritable bowel syndrome, interstitial cystitis/painful bladder syndrome, fibromyalgia, endometriosis, chronic tension-type and migraine headache and chronic low back pain.
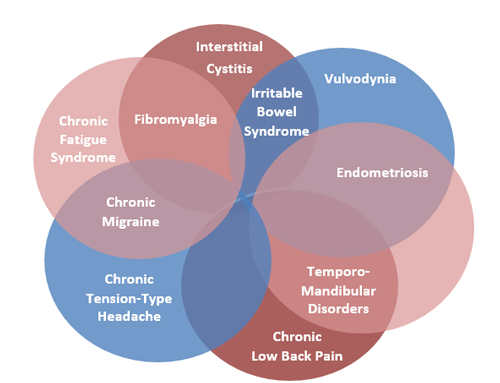
The complexity of overlap among COPCs is demonstrated in this figure. Any combination of conditions is possible. Some people may develop two disorders– either simultaneously or over the course of their lives – while others may develop three or more.
A growing number of studies (mostly conducted in clinic-based populations) demonstrate variable rates of overlap among COPCs, as well as increased risk of developing a new, different COPC as the number of pain conditions a person has increases.
Cumulative evidence suggests that there is often a delay in accurate diagnosis and effective treatment for individuals with COPCs, which can have serious consequences including worsening of site-specific and body-wide symptoms. This then makes COPCs more difficult to effectively treat, leading to a vicious cycle, with poorer health outcomes, diminished quality of life and increased disability.
Compared to healthy individuals, those with COPCs report enhanced pain perception, both increased pain intensity and lower sensory and pain thresholds, with the application of a variety of sensory stimuli (e.g., pressure, thermal, vibratory, electrical). These sensitivities are found not only at the body site where a person experiences chronic pain, but at remote locations, such as the thumb, shin and arm.
Recent studies, including those utilizing functional MRI, also provide evidence that other sensory input, such as light, sound and odor, are biologically amplified in patients with COPCs. In these studies, the insula – the brain region that plays a critical role in sensory integration – most consistently shows hyperactivity.
This blog highlights some of the key findings in patients with COPCs, which are consistent with what I see in my clinical practice. Recently, I worked with 2 Freedom clients who came to me for evaluation and treatment of a potential TMD. With further inquiry and testing, we found they had coexisting chronic pain conditions in conjunction with TMD. One of the good fortunes or luxuries we have at Freedom is the ability to co- treat with other health care professionals in house. We employ specialists who treat all of the COPCs mentioned in this article. In this recent example, it was determined that my 2 clients would also benefit from the expertise of our Women’s Health Experts. I firmly believe Freedom offers an invaluable resource for patients suffering from COPCs who elsewhere could not find relief. We regularly hear from our patients that in previous care the dots were never connected, leading to pain escalation, invalidation and frustration with the healthcare system. Fortunately, our team of experts have the skills and desire to help COPC patients find answers and relief.
I recently completed a course entitled: Preventing Chronic Pain: A Human Systems Approach. This course provided a great summary on how individual risk factors in the areas of cognitive, behavioral, physical, emotional, spiritual, social, and environmental health impact chronic pain. In my practice I see how strongly they influence my patient’s prognosis. I find it valuable to combine the human systems approach with evidence-based self-management strategies which empower patients to reduce and prevent chronic pain.
At Freedom we focus on overall health and wellness. We are committed to providing our clients with the highest standard of care, including a multifaceted, in house approach for COPCs. If you are suffering from chronic pain, we would welcome the opportunity to be a part of your healing process. Even better, visit us before your pain becomes chronic! I always say to my clients, “small problem, small fix, quicker recovery…. Big problem, requires a bigger, more comprehensive fix, and takes significant longer to recover from!”

